Healthcare payments plumbing - (Part 1)
837, 835 and other jargon in administrative transactions
Find me on LinkedIn @tejasinamdar, Twitter @tejasinamdar_, and tejasinamdar.com.
Administrative and billing expenses account for as much as 30% of all healthcare costs. Anyone looking to bend the cost curve must look at the inefficiencies and hidden costs in revenue cycle management. Before looking at the inefficiencies, let’s look at how things work today. The relationship between healthcare payers and providers revolves around two types of transactions - administrative and financial. The former is primarily informational and the latter is all about the operational mechanics of moving money from one account to another. Administrative transactions include eligibility, claims, claims status, remittance, denials etc. Financial transactions include the actions involved in transferring money - cash, check, credit/debit cards, automated clearing house (ACH) and other electronic methods etc. The activities related to managing these two transactions are referred to as the revenue cycle.
Starting 2014, Congress required Health Insurance Portability and Accountability Act (HIPAA)-covered entities—health plans, clearinghouses, and covered health care providers to adopt practices in line with “Administrative Simplification”. These practices require compliance with operating rules of Electronic Data Interchange (EDI) Transaction Sets and Electronic Funds Transfer (EFT). This series of posts takes a high level look at these administrative transaction sets in part 1, the current landscape of B2B payments in part 2 and how cost shifting from traditional payers to patients is affecting this payments landscape in part 3.
There are four main organizations in charge of developing and maintaining healthcare transaction standards:
Accredited Standards Committee (ASC) X12 - Responsible for EDI codes used in healthcare administrative transactions. Covered in Part 1
The Electronic Payments Association (NACHA) - Responsible for operating rules for all financial transactions via ACH network - including EFT transactions in healthcare. Covered in Part 2.
Health Level 7 (HL7) - Responsible for standards related to exchange of clinical health information used in electronic health records etc. There is a lot of activity in this space right now with CMS mandated interoperability and patient access rules. This topic is for a dedicated post on its own.
National Council for Prescription Drug Programs (NCPDP) - Responsible for EDI standards used by the retail pharmacy industry.
The first two are most relevant to healthcare payments plumbing and those are the standards we will focus on in this series of posts.
One common language for administrative transactions
Imagine every plan sponsor, payer and provider using their own format to communicate with each other. It would be a nightmare and would be wildly inefficient. The Health Insurance Portability and Accountability Act (HIPAA) mandated the adoption of standards for electronic transactions to simplify administrative transactions. The standards adopted for Electronic Data Interchange (EDI) are set by Accredited Standards Committee (ASC) X12. You will most commonly read or hear about these EDI transactions simply being referred to by their numbers. 837 and 835 are talked about all the time as medical claims data is used across the board by all sorts of entities to understand utilization of healthcare services.
Here’s what all those numbers mean -
834 - Benefit enrollment and maintenance - Enrollment or termination information passed from a plan sponsor (like an employer) to the health plan conveying information like - New enrollments, changes in a member’s enrollment, reinstatement of a member’s enrollment, dis-enrollment of members (i.e., termination of plan membership)
820 - Payment order/remittance advice - Information shared with health plan about healthcare premiums, payment processing (payroll deductions etc.) for individuals being covered by the health plan.
270 - Eligibility, coverage, or benefit inquiry - This transaction is used by providers to request information from the health plan about deductibles, co-pays, and coinsurance, coverage information for specific service types, provide secure access to eligibility information over the Internet, view the eligibility and benefits for the patient.
271 - Eligibility, coverage, or benefit information - This transaction is used by payers to respond to request for information from providers about the patients eligibility, coverage and benefits mentioned in 270. Health plans have to respond to these requests in real time.
278 - Health care service review information - There are times when health providers have to receive prior authorization from the patients health plan before they can deliver certain services and drugs or make a referral to another provider. This is the transaction used to get prior authorization.
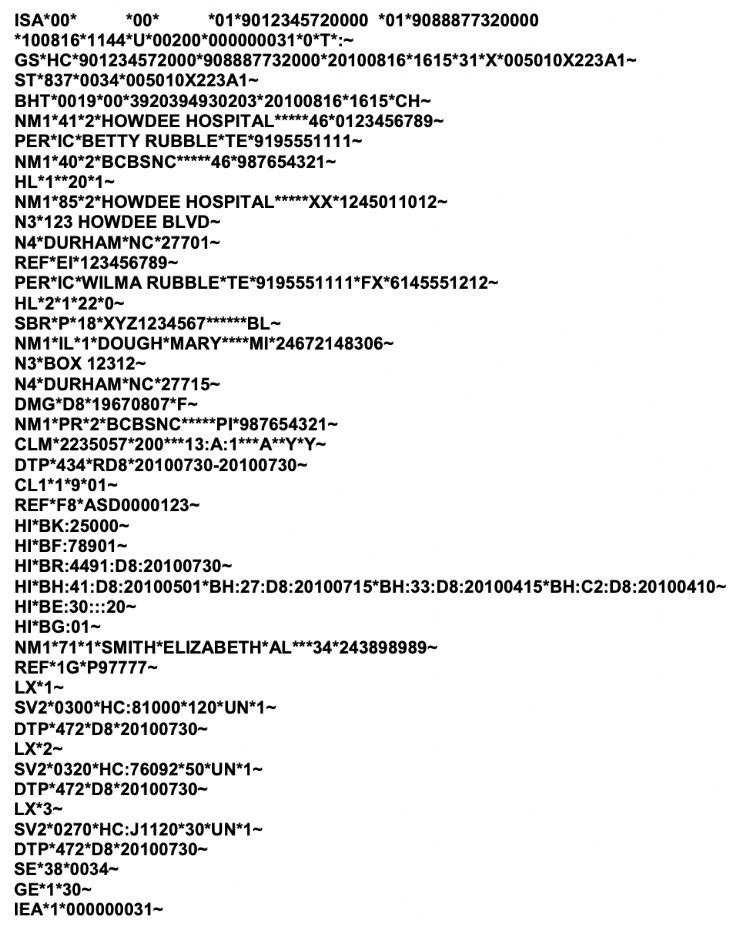
837 - Health care claim - Whenever a healthcare provider delivers care, they submit a request to the health plan to get paid. This claim contains detailed information about services delivered during the healthcare encounter, information about the patient, provider, payer etc. These claims get routed through a clearinghouse which checks the claims for errors and if approved submits to the payer so that a payment can be made to the provider. You can read more about clearinghouses here. Here’s what an 837 looks like. Part 1 of this newsletter discussed various medical codes. Those codes are what appear on the claim.
276 - Health care claim status request - It can take weeks and months to approve / deny a claim. This transaction is used by providers to check up on the status of submitted claims with the health plan.
277 - Health care claim status information - This transaction is used by payers to provide an update on the claim status requested, submitted as a 276, by the provider. It may come as a surprise that many claims never get followed up on or get rejected and are uncontested because they are not worth the hassle.
835 - Health care claim payment advice - When a claim is approved, the payer uses this transaction to complete the payment. This transaction takes two forms Electronic Remittance Advice (ERA) and Electronic Funds Transfer (EFT). ERA is essentially the explanation of benefits (the like the “THIS IS NOT A BILL” document we get months after a visit) from health plan to provider that provides information about contract agreements, secondary payers, benefits coverage, expected copays and co-insurance. EFT (more on this in part 2) is used by the health plan to direct its financial institution to make the payment to the provider. It includes things like amount, name, account number, routing number, date etc. Here’s what an 835 looks like.
To summarize, it takes all this just to confirm insurance coverage for a patient, communicate what care was delivered and get paid for it. Revenue cycle management is incredibly complex and simplifying any part of it is easier said than done. In part 2 we will take a look at how money is actually transferred from the payer to provider. In part 3, we will take a look at why providers are exploring alternative methods such as discounts for upfront payments, direct contracting, D2C healthcare etc. to eliminate the frustrations of collections from payers.
Do you know this space really well? Reach out or comment below and share where I got things right and where I got them wrong. Always open to feedback!
Thanks for reading hick-picks! If you enjoyed reading, please like, comment, share, and subscribe. You can find me on LinkedIn, Twitter, and tejasinamdar.com.